
Total hip replacement surgery is a safe, reliable procedure that can relieve your pain and stiffness and return you to most of the activities that you enjoy.
Degeneration of your hip joint has many different causes. With major advances in hip technology, the improvement in surgical outcome has vastly increased the use of hip replacement surgery in Australia.
Have a question about Total Hip Replacement Surgery.
People with hip joint damage that causes pain and interferes with daily activities despite trying other treatments such as exercise, walking aids and medication without significant improvement may be candidates for hip replacement surgery.
To diagnose degeneration in the hip joint, a complete history followed by physical examination is required. Your history is compiled by asking questions about your hip pain, medications you may be taking, and prior injury and other bone and joint problems you may have.
A physical examination will assess the range of motion in your hip. Observing how you walk, sit, bend and move will also assist in your assessment.

The prosthetic implant used in hip replacement procedures consist of different parts; the acetabular component, the femoral component and the articular interface. Options exist for different patients and indications. Correct selection of the prosthesis is important.
The Acetabular cup is the component which is placed into the acetabulum (hip socket). Cartilage and bone are removed from the acetabulum and the acetabular cup is attached using friction or cement. Like a healthy hip, your prosthesis has smooth gliding surfaces that allow you to move easily and without pain. Materials may vary, including steel, plastic (Polyethylene) or ceramic. Some acetabular cups are one piece, while others are modular. One piece (monobloc) shells are either polyethylene or metal, they have their articular surface machined on the inside surface of the cup and do not rely on a locking mechanism to hold a liner in place. A monobloc polyethylene cup is cemented in place while a metal cup is held in place by a metal coating on the outside of the cup. Modular cups consist of two pieces, a shell and liner. The shell is made of metal, the outside has a porous coating while the inside contains a locking mechanism designed to accept a liner.
The femoral component is the component that fits in the femur (thigh bone). Bone is removed and the femur is shaped to accept the femoral stem with attached prosthetic femoral head (ball). There are two types of fixation: cemented and uncemented. Cemented stems use acrylicbone cement to form a mantle between the stem and to the bone. Uncemented stems use friction, shape and surface coatings to stimulate bone to remodel and bond to the implant. Stems are made of multiple materials (titanium, cobalt chromium, stainless steel, and polymer composites) and they can be monolithic or modular. Modular components consist of different head dimensions and/or modular neck orientations; these attach via a taper similar to a Morse taper. These options allow for variability in leg length, offset and version. Femoral heads are made of metal or ceramic material. Metal heads, made of cobalt chromium for hardness, are machined to size and then polished to reduce wear of the socket liner. Ceramic heads are more smooth than polished metal heads, have a lower coefficient of friction than a cobalt chrome head.
There are four alternative articular interfaces that could be used:
Metal on Polyethylene – This is the traditional material which has been used for many years. There has been significant improvements in the polyethylene over the last 5 years. Ultra crossed linking of the molecules has dramatically reduced the wear of the polyethylene and this has allowed for larger ball heads to be used. With larger balled heads the risk of hip dislocation has been shown to be significantly reduced.
Ceramic on Polyethylene – There has been significant improvements in the polyethylene over the last 5 years. Ultra crossed linking of the molecules has dramatically reduced the wear of the polyethylene. Ceramic has a very low wear rate, it is however somewhat brittle in structure and there is a small but definite incidence of fracture of the ceramic.
Ceramic on Ceramic – This has a very low wear rate. It is also a very bioinert substance, in that the wear debris does not seem to cause significant problem either locally or elsewhere in the body. It is however somewhat brittle in structure, and there is a small but definite incidence of fracture of the ceramic. If this occurs it requires urgent revision of the articulating surfaces.
The other bearing surface is Metal on Metal which Professor Kohan does not use. Recent studies have shown that metal-on-metal devices may have problems. This is by no means universal, and there are some well functioning, well-established, durable implants which have been used and continue to be used. Metal on metal devices have been used for over 40 years in patients with high activity levels. However, some recent implants, have proved unsatisfactory, and have been withdrawn from the market. Hip resurfacing surgery at this stage can only be carried out with metal on metal implants. The metal on metal implants which are currently used have a long track record of durable, consistent, and reliable function. However, being mindful of the recent problems being attributed to metallic implants, in this practice we only use these bearings under specific circumstances, which will be discussed in detail with the patient at the time.

There are several ways for a surgeon to perform total hip replacement surgery including (but not limited to): posterior (Moore), lateral (Hardinge or Liverpool), antero-lateral (Watson-Jones), minimally invasive and The Direct Anterior (Hueter) AMIS® approaches.
Some approaches are more muscle sparing than others leading to a quicker recovery however the most important aspect of any hip surgery is to ensure that the prosthesis is implanted accurately and correctly, that the surgery is carried out in an efficient manner minimizing blood loss and reducing anaesthetic time and the risk of complications is kept to a minimum.
Immediately after hip replacement surgery, you will wake up in the recovery room. You may feel a bit groggy. Professor Kohan and his staff will monitor you, checking your blood pressure, temperature and pulse. Dr Kerr will also assess your pain level.
Post-operative x-rays will be performed in recovery and after 45 minutes – 1 hour you will then be transferred back to your room on the ward.
When you arrive to your room, you will have:
You will be out of bed and walking within 4 hours after surgery.
On the first day after surgery you will learn to walk up and down stairs with a physiotherapist at the hospital. The pace at which you regain agility on stairs depends on individual traits. This is the day you will also go home.
In the first week following surgery you may experience:
From your thigh down into your foot is common. This at times may be quite marked. The swelling will increase for the first few days after surgery and will gradually diminish. Some swelling can be present for 12 months or so. The swelling may be diminished by walking as the muscle function will push the fluid away. When you stop walking, the limb should be elevated above the level of the hip.
Marked bruising can be found in some patients. This can be found from your thigh down into your foot. At times the bruising can be quite dramatic but it will resolve. It is the result of some residual bleeding making its way to the surface. The body will eventually remove the bruising. It is also the result of the blood thinning tablets you will be taking.The blood thinning tablets will tend to make the bleeding after surgery a little more marked because the blood clotting is impaired. This is however preferable to developing a blood clot.
On occasions blisters will develop near the operation and possibly above it. The blistering is due to surface fluid. It looks dramatic but it is of no consequence and always resolves. One cause may be the bandage rubbing on the skin. Sometimes, when the blood dries in the bandage it can be like cardboard and rub on the skin producing these blisters. We change the bandage after about a week but would prefer not to interfere with that earlier because of the risk of infection. After about a week the wound is sealed enough to be a reasonable barrier against infection. Another cause for the blistering is tissue swelling. This is associated with the bruising and is a result of fluid leaking into the skin. These blisters always go away. They may burst and leak fluid and again the appearance may be dramatic. Sometimes if they are large we may burst them. This is so that the dressings sit more comfortably.
Your muscles can feel stiff and sore to touch. During the operation some stretching and pulling of the muscles occurs. This may result in some pain like a corked thigh. Occasionally you may feel cramps and spasms. The discomfort however will resolve and activity such as walking, stretching, physiotherapy, etc, will help to speed the improvement.
The operated site may feel hot and the heat may last for 12 months. As part of the healing process the operation site requires more blood supply from the body and it is this extra blood supply which is the cause of the local heat.
For the first 2 weeks after surgery your activity level is usually limited however you will be able to walk independently, use the bathroom and perform normal activities of daily living. If you have had anterior surgery hip bending is not restricted.
After 2 weeks you will be able to engage in moderate activities, such as driving a car and climbing stairs.
Within 6 weeks you should be able to resume most of your normal activities. Complete surgical healing takes 6 – 8 weeks. During this time some swelling and discomfort is normal and should be manageable with the prescribed medication.
The fear of pain can interfere with a satisfactory recovery, and can interfere with a rapid return to normal function. Accordingly, a large part of the preoperative preparation revolves around an understanding of how we are going to manage the pain, and focusing on a rapid return to an active life.
The aim is to try and minimise the impact of the operation on the patient’s life.
The Joint Orthopaedic Centre have developed a multimodal technique for the control of pain following knee and hip surgery, called The Kohan-Kerr”Local Infiltration Analgesia Technique” (LIA).
LIA is based on systematic infiltration of a mixture of ropivacaine, ketorolac, and adrenaline into the tissues around the surgical field to achieve satisfactory pain control with little physiological disturbance.
The technique allows virtually immediate mobilization and earlier discharge from hospital.
In order to minimise the pain, we adopt three pathways.
There are precautions necessary to undertake after hip surgery and these vary according to the surgical technique used.
With the Posterior/Antrolateral Approaches precautions are as follows:
Do not cross your legs or ankles when you are sitting, standing, or lying down.

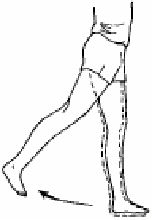
With the Anterior Approach, hip flexion is unlimited but hip extension needs to be restricted for a period of six weeks after your operation.
Do not do this hip extension exercise for 6 weeks following an AMIS Hip Replacement Procedure.
Do not bend too far forward from your waist or pull your leg up past your waist. This bending is called hip flexion.
As with all surgery there are certain risks and potential complications. Although the incidence of these risk factors is low each patient needs to be informed of the possible complications prior to surgery.
Over 95% of patients who have a hip replacement surgery have excellent relief of pain and improved mobility. Most patients never require a re-do of the hip replacement.
Infection is uncommon occurring in less than two percent of operations. It is usual for each patient to be is given intravenous antibiotics at the time of their joint surgery. However, this cannot possibly cover all types of infection which may be encountered. Infection in the postoperative period in most patients is treatable. It may require longer hospitalisation, treatment with antibiotics for a longer period than normal and washout of the joint. In some cases, the implant will be removed to treat the infection before reimplanting a new joint. In rare cases when the infection cannot be treated successfully, a patient may need to have the artificial joint removed permanently. Infection is uncommon and we take precautions to avoid this problem.Delayed infection has been reported years after joint replacement, and appears to be related to the ability of the implants, in general, to harbor bacteria transported by the blood stream from other sites of the body. Bladder or kidney infections can be a source but dental abscesses, infected ingrown toe nails, or skin infections may also be a significant danger to a joint implant. Please call the office, or contact your family doctor if infection is suspected in any area.
Please Note: If dental surgery, bladder surgery, bowel surgery or rectal surgery is planned, the physician or dentist should be informed that you have had a joint replacement.
Another potential risk is the occurrence of blood clot or thrombosis after a joint replacement. Because our patients are mobilised very soon after surgery, this potential risk is small. In addition to early mobilisation patients are treated with calf compressors to prevent Thromboembolic disease (the development of clots in the lower extremities) during surgery. Post surgery TED stockings and low doses of aspirin or other anticoagulation (blood thinners) medications are prescribed depending on the patient’s medical history. In patients without any history of thromboembolic problems we advise taking aspirin, 300 mg per day, for a period of six weeks.
These measures are in place to reduce the risk of forming a clot. In the event the patient is diagnosed with a blood clot intravenous or subcutaneous anticoagulation therapy may be required. However, some clots are small and of no clinical significance and so do not require any specific treatment other than the aspirin. This needs to be assessed on a case-by-case basis. If full anticoagulation is required however, this means a longer stay in hospital for the patient.
There is no perfect treatment and while trying to decrease the significant risk of deep vein thrombosis and the possibility of more serious complications such as pulmonary embolism (blood clots breaking off and traveling to the lungs), other potential side effects (such as bleeding) can occur with the drugs used to decrease this complication. These medications require extreme care in their use.
Every endeavor is made to maintain the legs at equal leg length, however, sometimes the leg can be slightly lengthened as a result of the hip replacement. Usually, a hip joint which is diseased enough to require replacement is stiff. It may also be a little short, because of deformity, wear or destruction of the bony surfaces which rub together. After surgery, the operated side almost always feels longer. This feeling gradually diminishes with increasing use, strengthening, and my ability, over a period of 12 months or so. Although we take measures to try and ensure limb length remains unchanged, or on some occasions, is modified to try and achieve limb length equality, generally, we can get only to within a centimetre or so of limb equality. Generally, this is not enough to cause a limp. On occasions, however, a small shoe raise adjustment may be required.
Nerve damage is another potential risk factor when considering joint replacement surgery. The nerves can be traumatised at the time of the operation through stretching and occasionally due to postoperative swelling. Precautions are in place to protect the nerves via superior surgical technique but the risk nevertheless, exists for these potential complications to occur. The risk factors are small and are dependant on the age and prior medical condition of the patient.
Diabetes, smoking and peripheral vascular disease are risk factors, as is the presence of previous back problems.
If nerve damage occurs rest and further examination of the nerve will be required and possible further surgery.
A fracture may occur at the level of the neck of the femur, below the femoral component. The fracture may occur during the operation when the femoral head is being prepared to receive the component or it may occur later, as a result of excessive loading in the postoperative period. We try and minimise the impact of this complication by assessing the strength of the bone before the operation with a bone mineral density investigation and by trying to limit the activity postoperatively.
A small percentage of patients require revision surgery because of excessive wear of the ball and socket joint or loosening of the prosthesis. This may cause pain and a limp, and the diagnosis can be confirmed with x-rays. Excessive wear of the ball and socket joint is one of the most common reasons why revision hip surgery is performed.
A decrease in motion of a joint is also a potential risk. The joint condition prior to surgery will have some bearing on the movement post surgery. On occasions, excessive bone can form postoperatively, that can limit the range of movement. This excessive bone formation cannot be totally predictable, but, if it has happened at another joint replacement site, the risk is increased. The risk is also greater in men, and over the age of 70. Physiotherapy and exercise are encouraged prior to surgery. Post surgery, if the joint remains stiff, physiotherapy or manipulation can improve the range of motion in the joint.
Other complications that can occur include, instrument failure and breakage, muscle wasting, artery or vein trauma, drug reactions, implant breakage and loss of income, through prolonged hospitalisation, and a longer than anticipated recovery. Potential medical risks are also many and varied. They can range from minor to more serious complications. These may include cardiovascular, (Heart attack), respiratory, gastrointestinal, neurological (stroke) and genitourinary systems in the body. The general health of a patient undertaking surgery is an important factor. Many patients who need hip replacement surgery are elderly, with multiple other problems. These problems may add to the risks in undertaking surgery of this type.
While orthopaedic surgery carries with it certain risks, it would be safe to say that these risks can be encountered with any surgical procedure. Careful pre-surgical screening and education, a careful surgical technique and a closely monitored postoperative period all add up to minimising the occurrence of any of these complications. It is our conscientious effort to adhere to these criteria whenever a patient is under our care. With this in mind, the potential for a complication to occur is reduced.
Generally our ‘Estimate of Fees’ is accurate however, on occasion unforeseen circumstances can arise during the operation which may require additional medical services or a different, more costly prosthetic device to be used. If this happens there may be additional costs to you that are not covered by the estimate.
This will be fully explained to you after the operation should it occur.
Professor Kohan’s Surgical Fees
Medical Item No: 49318
Surgical Assistant Fees
The surgical assistant fees will either be billed to you directly or Professor Kohan will bill you on his behalf.
Medicare Item No: 51303
Anesthetic Fees
You will meet with Dr Kerr, the anesthetist before your operation so that you can obtain an estimate of his fees. These will be billed to you directly.
Medical Item No’s : 17620, 17690, 21214, 23111, 22045, 18225
There will be 2 ‘no charge’ consultations after your Total Hip Replacement procedure.
Aftercare appointments with Professor Kohan following your procedure include:
7 Days Post Surgery – This appointment is in order to check the skin cut & for Professor Kohan to asses your overall recovery.
14 Days Post Surgery – At this appointment the skin clips will be removed. An ultrasound will also be done by our radiographer in the rooms in order for Professor Kohan to check for blood clots.
6 Weeks Post Surgery – At this appointment Professor Kohan will asses the X-ray and monitor your overall recovery.
Consultations after this time attract a fee which is reimbursed in part from Medicare.
These fees should be discussed with the hospital directly. Please be sure to check with your health fund regarding a gap or out of pocket expenses.
If you are privately insured the prosthesis used in a Total Hip Replacement procedure is usually fully covered by your Health fund.
These fees are payable directly to the sonographer.

Dr. Farah’s specialty interests are hip and knee surgery, hip and knee arthroplasty (joint replacement), anterior minimally invasive hip replacement and sports knee surgery.