Menu
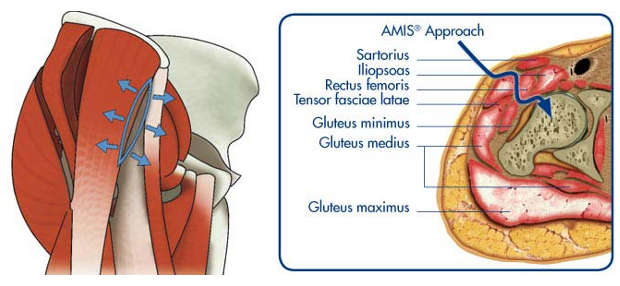
AMIS® (Anterior Minimally Invasive Surgery) however, is a surgical technique used in total hip replacement procedures which follows an inter-muscular and inter-nervous plane to reduce the risk of injury to muscles, tendons, vessels and nerves. By respecting the nerves and because no muscles are cut this aids in rapid recovery for patients following surgery.
The anterior approach to the hip joint was first described by a German surgeon Dr Hueter in 1881. It was initially used for draining infected joints.
French surgeons used the anterior approach with the first total hip replacements in 1949 and continue up to the present day.
Prof. Frederick Laude in Paris adapted the approach 12 years ago and modified the traction table and tissue retractors used in the operating room to create a truly “minimally invasive approach” to the hip for joint replacement. His approach was termed AMIS® (Anterior Minimally Invasive Surgery).
When having a hip replacement a very important consideration is the method used by your surgeon to insert the artificial joint. A Direct Anterior Approach (AMIS®) is a method of inserting the artificial joint through the front (ie. anterior) without cutting any muscles or damaging nerves. All other common approaches (ie. lateral and posterior) involve cutting muscles or tendons.
The procedure is performed in hospital as an inpatient. This means that the hospital stay is usually overnight but may be longer, depending on your individual circumstances. The operation will take approximately 1.5 hours.
The incision is approximately 7 -10 cm long. The incision is made over the top of your hip joint in the region of your groin. The worn surfaces of the hip are removed and the surfaces are replaced with artificial components. Metal is used for all components however the bearing surfaces may vary depending on the circumstances: metal, ceramic, or plastic.
Ligaments and tendons are preserved so it is possible following a primary joint replacement to walk a few hours after surgery, fully weight-bearing on your new hip. In fact, it is something that we want you to do unless otherwise advised. At the site of the operation the tissues may not be completely flat immediately after surgery because of some swelling. This will however settle down a few weeks after surgery.
The anaesthetic service is provided by Dr Dennis Kerr. He will discuss your anaesthetic and pain control at a consultation before your surgery. It is essential that you see Dr. Kerr in preparation for the operation and that your spouse, partner, or significant other person in your life come to the consultation as well. The importance of this consultation cannot be overemphasised.
Click on the Video below for a step by step guide on the AMIS® surgical technique:
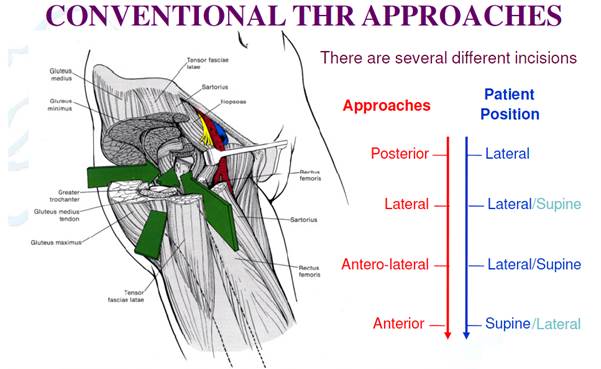
Conventional – Antero-lateral
In the conventional-antero-lateral approach the hip abductor (gluteus medius and minimis) muscles/tendons are detached and split, frequently resulting in a permanent limp as they are unable to stabilise the hip after the operation. Bone lumps often grow in the damaged gluteus muscle. This apprach also cuts through the tendons of gluteus maximus and tensor fascia lata muscles.
Conventional – Posterior
In the conventional-posterior approach the gluteus minimis muscle is cut off the capsule often resulting in lumps of bone growing in the muscle after the operation. This approach has the highest risk of dislocation but there is usually no limp after surgery. The posterior approach also cuts through the tendons of gluteus maximus, tensor fascia lata, piriformis, gemelli and obturator muscles.
AMIS® Approach
The AMIS® incision is only 7-10cm in length, whereas antero-lateral or posterior approach incisions are usually between 15-30cm in length!
With AMIS® there is no detachment, splitting or denervation of muscle. No muscles or tendons are cut as they are simply retracted to create a gap. The tensor fascia lata muscle is retracted laterally whilst the rectus femoris muscle is retracted medially. There is no gluteal (buttock) muscle injury with this approach.
The gluteal muscles provide the main hip power and stability and as they are entirely intact with the AMIS® approach a faster recovery is expected. The posterior or antero-lateral approaches cut through the buttock muscles and tendons even when they are so-called mini-incisions or mini-invasive operations.
The AMIS® approach enters between the nerve supply to the muscles so the muscle fibres retain their full ability to function after the operation. Other approaches permanently damage either muscle fibres and/or the nerves which supply them so there may be a permanent loss of nerve function and/or partial muscle wasting.
Remember that ALL approaches if performed correctly will result in a successful pain free outcome that should last at least 20-30 years using modern day implants.
AMIS® can potentially provide you with the following benefits:
DECREASED POST-OPERATIVE PAIN
In comparison with “conventional” surgical techniques, the AMIS approach can reduce the post-operative pain as muscles are not cut.
SHORTER REHABILITATION
Rehabilitation can usually start the day of the operation or the day after, subject to your doctor’s approval, based on your post-operative conditions. Standing up and walking with arm crutches can start immediately, with your doctor’s authorisation as well.
SHORTER HOSPITAL STAY
The AMIS® technique usually significantly reduces the duration of hospital stay. Your surgeon may still recommend you a longer stay depending on your post-operative condition.
SMALL SKIN SCAR
With AMIS®, the skin incision is often shorter than with “conventional” surgery and therefore scar tissue is reduced.
FASTER RETURN TO DAILY ACTIVITIES
The AMIS® technique allows you to return to daily activities in a shorter time frame.
LESS BLOOD LOSS
Preservation of muscles and vessels potentially reduces blood loss. Transfusions are rare, blood clots in the legs (deep venous thrombosis) are potentially less likely.
REDUCED RISK OF DISLOCATION
(separation of the hip ball and socket)
As a result of the AMIS® technique the preservation of muscles significantly improves the stability of the hip. The risk of dislocation is minimal and the post-operative limitation of movements, usually prescribed in other techniques, is not necessary. The risk of dislocation is reduced because the anterior approach is performed from the front of your body and dislocation is mainly related to posterior hip structure damage.
PREVENTION OF LIMPING
AMIS® is characterised by a surgical technique that protects the various muscles, blood vessels and nerves encountered during exposure of the hip joint. Minimizing muscle and nerve damage reduces the chances of limping.
You may drive when able to get in and out of the car comfortably, have excellent control of your legs and are not taking pain medications.
Depending on your general condition and only with approval from your surgeon, you may be driving in 8 -10 days.
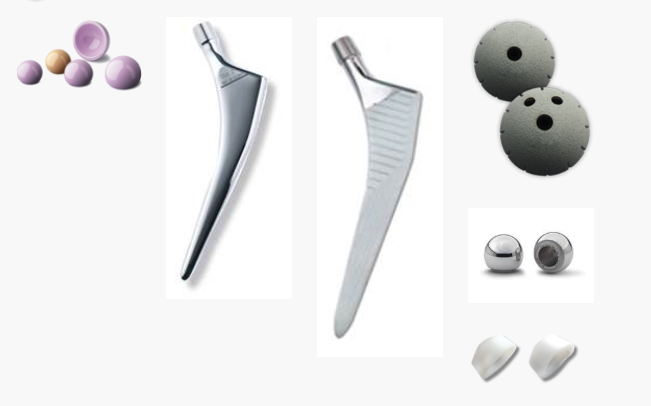
The prosthetic implant used in hip replacement procedures consist of different parts; the acetabular component, the femoral component and the articular interface. Options exist for different patients and indications. Correct selection of the prosthesis is important.
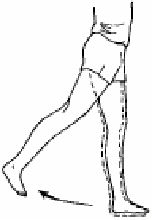
There are precautions necessary to undertake after hip surgery. The major precaution is limiting hip extension. This is different from most hip replacement procedures which are done from the back and limit flexion.
With the anterior approach, hip flexion is unlimited but hip extension needs to be restricted for a period of six weeks after your operation.
Do not do this hip extension exercise for 6 weeks following surgery.
How long will my leg continue to swell and hurt?
The pain usually decreases rapidly during the first few weeks but the pain continues to improve for 12 months or even longer. The swelling is due to alterations in fluid return up the limb and will gradually diminish but may take 12 months or longer. Mobilisation helps. Exercise, stockings and elevation also help.
How much exercise should I do and how can I tell if I have done too much?
Mild and moderate exercise is beneficial but over-exercise is painful and possibly harmful. Generally the more active you are the better, but within limits.
When can I drive?
Driving is an individual matter. Some people regain their co-ordination and reflexes quickly and others take longer. Following hip surgery you should avoid driving for at least 2 to 3 weeks depending on your progress. Driving should not be considered if you are still taking pain medication.
When will I be able to go up and down stairs?
On the first day after surgery you should learn to walk up and down stairs with a physiotherapist at the hospital. The pace at which you regain agility on stairs depends on individual traits.
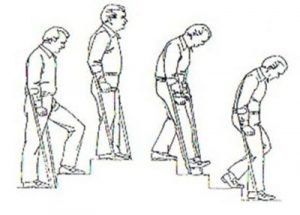
Up stairs: Take a step up with your good leg, then take the operated leg, followed by crutch or stick.
Down stairs: Place your crutch or stick first, then take a step down with the operated leg, followed by the good leg. Always go one step at a time.
What kind of shoes should I wear?
High heels should be avoided for the first 3 months otherwise there are no rules regarding shoes.
Should I use a heating pad or ice packs?
Both ice and heat can be used to help relieve pain but both can be harmful if left on too long. Never sleep with a heating pad on your hip as it can damage the skin and even cause a severe burn. Ice can be used several times a day. 20 minutes on and 20 minutes off is the usual regime.
How long should I continue taking my medications after surgery?
If iron is prescribed, it should be continued for 1 month after discharge from the hospital. Blood thinning medications (Aspirin) should be taken for 6 weeks. All pain medications may be taken as directed for pain. If you have any questions about your medications please ask.
Why do I have trouble sleeping at night?
Sleeping trouble is the most common question. You need patience. Surgical heeling takes approximately 6-8 weeks. Therefore you may be slightly uncomfortable for this time. Taking prescribed medication and applying ice can help. Also getting out of bed and moving the joint sometimes helps too.
Why don’t my legs feel equal in length?
This is a very commonly asked question. There are many reasons why you may feel a limb length discrepancy. During surgery, we used several methods to ensure limb length inequality, as best we can. Given current technology, probably, plus or -1 cm is about as accurate as we can get. Generally speaking, though, you need at least 1/2 cm or more before a permanent limp develops. This is because the spine of the pelvis can usually accommodate for the limb length inequality.
Another reason is that, before surgery, the hip is quite stiff. Over the years, you have gradually adapted to the stiff hip, by altering the angle of your pelvis and the spine. That is the new “” normal”” length with which you going to surgery. After the surgery, much of the stiffness is immediately resolved, and the limb can now extend fully giving you the feeling that it is longer. It feels longer, but in fact the length is the same as it was before surgery, it is just able to be extended fully.
We usually advise that you adopt a wait and see approach. Simply using the leg, walking, and gentle exercises as advised will allow the body skeletal system to adapt. This may take a year. However, if you use shoe raises, or insoles to make up for the perceived inequality, the body does not have a chance to adapt.

Dr. Farah’s specialty interests are hip and knee surgery, hip and knee arthroplasty (joint replacement), anterior minimally invasive hip replacement and sports knee surgery.